The Gordon Center Team Discusses Stroke Education
Posted on May 31st, 2024May is National Stroke Awareness Month, a time to raise awareness about the symptoms and risk factors of stroke.

May is National Stroke Awareness Month, a time to raise awareness about the symptoms and risk factors of stroke.

Join us in acknowledging the individuals who are responsible for EMS training at the Gordon Center.

The use of standardized patients allows students to practice taking medical history on patients, doing physical exams and talking to patients. Read the Miami Today’s story featuring Dr. Gauri Agarwal, associate dean for curriculum at the University of Miami Miller School of Medicine and Gordon Center’s Samantha Syms, director of the Standardized Patient Program. Read Article

Dr. Barry Issenberg, recently shared profound insights on the future of patient simulation in One Million Lives, a Laerdal Podcast. In this podcast episode, Dr. Issenberg delves into the evolving landscape of patient simulation and its critical role in healthcare. For healthcare professionals eager to explore the transformative potential of patient simulation, this podcast is a must-listen.
Come join us at the 2023 NAVRA, for an in-person event showcasing the power of Point of Care Ultrasound in Trauma by the University of Miami Gordon Center.
In recent years, the use of point of care emergency ultrasound (POCUS) has become a rapidly growing field. In emergency medicine, US has been integrated for rapid diagnostic and procedural capabilities. There is increasing evidence that US has a role in out-of-hospital emergency care and with the advent of lower cost portable devices, the use of US in EMS is growing. Prehospital Ultrasound may be beneficial in the diagnosis and management of trauma and critically ill patients. EMS providers, with the appropriate training, can acquire and interpret ultrasound images and address prehospital diagnosis in real-time.

In what some are calling the next iteration of the internet, the metaverse is an unfamiliar digital world where you could be an avatar navigating computer-generated places and interacting with others in real time. In this space, the constraints of our physical, bricks and mortar world and travel habits fade. And new opportunities and challenges emerge.
At the University of Connecticut Health in Farmington, doctors in training got a first taste of what life could be like in a futuristic place like this when residents were given virtual reality headsets for the first time.
In a historic moment, orthopedic surgeries were largely put on hold because of the COVID-19 pandemic, says Olga Solovyova, MD, assistant professor of orthopedic surgery at UConn Health.
Now, residents put on goggles and see their avatars (digital representations of themselves) in a virtual operating room with a table, instruments and a virtual patient. They manipulate the instruments with controllers and feel the resistance when they saw or drill a bone and they feel the pressure drop when they cut through completely.
In VR, they can also peel away virtual layers of skin and muscle to better view the bone underneath. Training modules give feedback on how well students complete procedures and track their progress.
“Classically it was always the ‘see one; do one; teach one,’ mentality, watching first and then practicing then teaching others,” Solovyova says. Now residents can practice on their own repeatedly in a safe environment with professional feedback.
It also allows practicing rare surgeries that might not come up in real-life patients, Solovyova says.
Such training in digital environments like the metaverse is starting to become more common at other surgical residency programs in the U.S., she says.
Some aspects of the metaverse – a term just beginning to make its way into conversations – are already here like VR training, telemedicine and 3D printing.
Facebook’s announcement last year that it would be rebranded as Meta set off ripples of curiosity about the concept. Definitions differ, but at its core the metaverse is the space where VR, augmented reality, artificial intelligence, the Internet of Things (where unrelated devices communicate with each other), quantum computing and several other technologies come together to bridge the physical and digital worlds.
A report by industry trends analyst Gartner predicts that 25% of people in the world will spend at least an hour a day in the metaverse by 2026, whether for work, shopping, education or entertainment.
And with the wearable technology today, people can monitor their vitals and update their doctor with real-time data. Barry Issenberg, MD, director of the Gordon Center for Simulation and Innovation in Medical Education at the University of Miami, says electronic health records in the metaverse will likely become living documents updated from sensors in clothing or furniture, on phone apps or wearable devices.
Instead of people coming into a doctor’s office to be examined and have lab values interpreted, doctors will already have much of the picture in uploaded data.
That, he says, will help address a common complaint that with electronic health records medical visits have become strained with doctors distracted by typing information into templates.
Doctors can also set parameters for abnormalities so that if a patient’s blood pressure gets too high or walking abnormalities are detected, the doctor will be notified, enabling more proactive, preventative care.
Because people will also get the information in real time, they can become more engaged in their own care, Issenberg says.
In Miami, clinicians are working with emergency responders in the community using virtual tools. They can show a learner using a stethoscope, for instance, the anatomy that lies underneath the chest so the responders don’t have to imagine a hea
rt pumping — they can see it on a screen while hearing the sounds.
At Miami’s Bascom-Palmer Eye Institute, Issenberg says, a doctor developed personal goggles that can detect the visual response of patients. The goggles are sent to patients with vision problems so doctors can conduct exams without the patient having to come into the center.
A major stumbling block for ushering in the metaverse is a problem that has thwarted progress in the use of electronic health records, too. Health systems use different technologies that often don’t talk to each other.
The metaverse will find more seamless connectivity in large, contained systems such as the Veterans Administration, Kaiser Permanente and the Mayo Clinic, Issenberg says.
And clinical trial recruitment, patient engagement and monitoring could also look different in the metaverse, says Nimita Limaye, PhD, research vice president of Life Sciences R&D Strategy at International Data Corp., headquartered in Needham, MA.
Many of the challenges associated with clinical trials include a big burden on patients, which can result in people not following directions or dropping out of trials. Questionnaires can be long and difficult to fill out.
Virtual assistants could issue reminders on medications, ask patients how they are feeling each day, read questions to people and record the answers for investigators.
“I don’t think that’s very far away,” Limaye says, noting that voice commands are much more convenient than downloading and using apps, especially for older people who may have poor eyesight.
Amazon Web Services is already working with its voice and Chatbot solutions, Alexa and Amazon Lex, to improve clinical trial participation, reduce dropout rates and improve the quality of the data recorded.
One day, Limaye says, people with a particular disease or condition could ask a virtual assistant such as Alexa what clinical trials are available for them.
Exclusion and inclusion criteria could be built into the technology and the virtual assistant could answer with a list of trials and directions on how to sign up.
COVID-19 Limaye says, already changed clinical trials and made it more common for people to participate from home through telehealth, home health nurses, wearables and the direct-to-patient shipment of drugs and devices.
“The life sciences industry saw the proof of concept that technology can work with clinical trials,” she says.
As technologies advance, Limaye adds, equitable access will be critical.
While few can afford a sophisticated virtual reality headset yet, she points out, other solutions may be more widely accessible.

25th Anniversary of the First There First Care Conference & Gathering of Eagles
Honoring the Past, Connecting the Present, Developing the Future.
Seminole Hard Rock Hotel & Casino
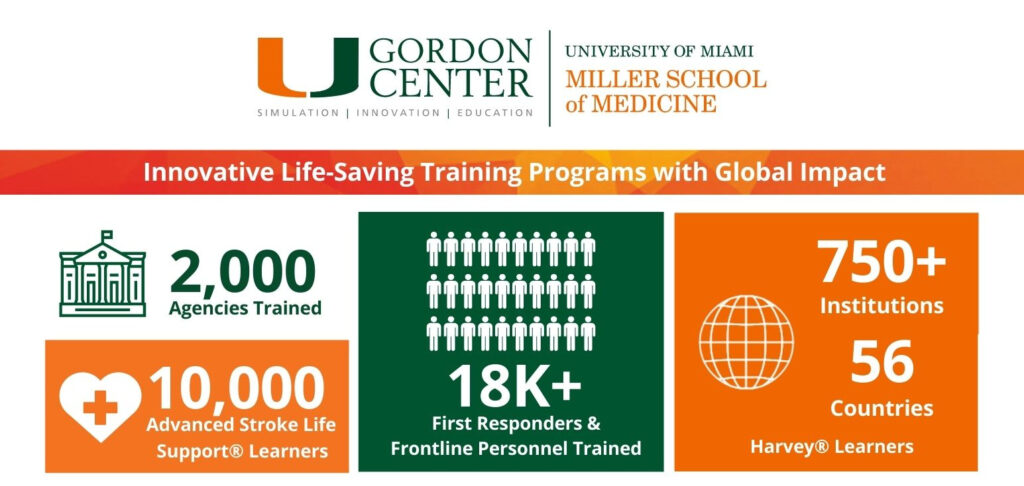
Our 2021 Annual Report is now available! Join us in looking back and learning about our plans going forward.

Don’t worry, you can experience all the Sim Week 2020 Streams right here!